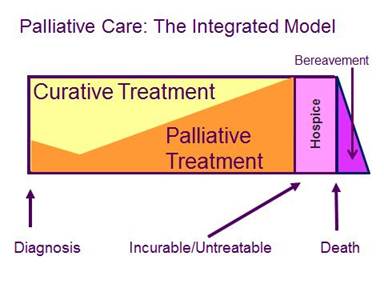
When Is It Time to Consider Palliative Care? Palliative medicine consultants often receive requests from colleagues to see a patient who is finally “ready to go palliative.” Sometimes it means that a patient wants to know more about hospice. Other times, it means that the patient’s family is concerned about the patient’s suffering, and wants more attention paid to pain and symptom management. Many times, providers aren’t quite sure how to help a patient with serious illness who is struggling with the current treatment plan and is not sure what other options exist. While hospice as a model of care, and as an insurance benefit, has been in existence in this country since the early 1980s, palliative care is a relatively new specialty (board certification through the American Board of Medical Specialties became official in 2008). Moreover, the vast majority of the American public has never heard of palliative medicine. Until recently, it was not a topic that was discussed until the very late stages of illness. Palliative care refers to the active, total care of patients with life-limiting illness, with a focus on relieving or preventing suffering – in all of its forms – related to the underlying illness or related to treatment of the illness. Examples of “life-limiting illness” include COPD, heart failure, dementia and cancer. Palliative care may be provided at any stage of a life-threatening illness. Importantly, patients can receive palliative care concurrently with disease-modifying care, and it is not limited to a particular diagnosis (like cancer) or prognosis. Palliative care typically encompasses symptom management, including both physical (such as pain, nausea, constipation, breathlessness, fatigue) and psychosocial (including delirium, anxiety, depression, spiritual distress) symptoms. Because suffering is typically so multidimensional, excellent palliative care is usually provided by interdisciplinary teams of providers including physicians, nurses, social workers, chaplains and other allied clinicians. Figure: Integrated Model Concurrent Palliative Care A patient is eligible for hospice when the prognosis is thought to be (given the expected course of illness) six months or less and the patient has decided to forego further treatment to cure the underlying life-threatening condition (they may still receive treatment for any other illness not related to the terminal condition). A patient must elect to enroll in hospice and must give consent to enroll. Table: Comparing Palliative Care and Hospice*
*The description of what benefits may be available for the care noted above is not a guarantee of benefits. Members should refer to their certificate of coverage to determine what, if any, benefits are available and more details regarding terms, conditions, limitations and exclusions. It is never too early to “go palliative.” Whenever a potentially life-threatening illness is affecting a patient’s quality of life, it is time to consider adding palliative care to the treatment plan. If available, an expert palliative care team can help manage symptoms, coordinate care and facilitate complex decision-making planning that may include preparing for end-of-life care, even if it may be months or years away. Dr. Eytan Szmuilowicz, director of the Section of Palliative Care at Northwestern University Feinberg School of Medicine, has provided this information about palliative care for Blue Review readers. |